Globally, 52 million children suffer from acute malnutrition. Children with moderate acute malnutrition are 3.4 times more likely to die than well-nourished children, and those with severe acute malnutrition are 11.6 times more likely. Acute malnutrition kills 875,000 children under the age of five annually.
The introduction a decade ago of Community-based Management of Acute Malnutrition (CMAM) made the screening and treatment of children with severe acute malnutrition more accessible: Community health workers, often volunteers (CHVs), conduct first-line screening and refer cases to a health facility for treatment. Children with severe acute malnutrition (and in some countries, children with moderate acute malnutrition) but without medical complications are treated through an outpatient program using energy-dense supplements that provide all necessary micronutrients.
Yet two key barriers limit the effectiveness of CMAM: Low participation in screening and low uptake and adherence to treatment.
The PROMIS program
The Innovative Approaches for the Prevention of Childhood Malnutrition (PROMIS) program, implemented by Helen Keller International between 2014 and 2017 in Burkina Faso, Mali, and Senegal, integrated preventive interventions into acute malnutrition (AM) screening. The preventive interventions aimed to prevent the occurrence of new cases of AM through the provision of dietary supplements (small quantity lipid-based nutrient supplements, or SQ-LNS) providing essential nutrients and through behavior change communication (BCC) on nutrition, health, and hygiene practices. The nutritional supplement was expected to serve as an incentive for caregivers to bring their children to AM screening sessions and as a result to increase referral, enrollment in, and completion of CMAM treatment.
To evaluate PROMIS’s impact, IFPRI conducted cluster-randomized controlled trials in Burkina Faso and Mali. A combined longitudinal and cross-sectional study design allowed us to assess impacts on both the incidence (longitudinal) and prevalence (cross-sectional) of acute malnutrition. In both countries, clusters (health center service areas) were randomly allocated to either the PROMIS intervention or a comparison study group.
The intervention
PROMIS’s preventive interventions (BCC and SQ-LNS) were offered at monthly screenings to all children in the intervention group who were younger than 2 years of age (and 6 months or older for SQ-LNS).
In Burkina Faso, the intervention was offered through preventive well-baby consultations organized by primary healthcare centers (health facility platform). Caregivers from both the intervention and comparison groups with children aged 0–23 months were invited to attend monthly consultations. At the end of the sessions, caregivers from the intervention group were given an enhanced form of BCC and a monthly supply of SQ-LNS (for children 6-23 months of age).
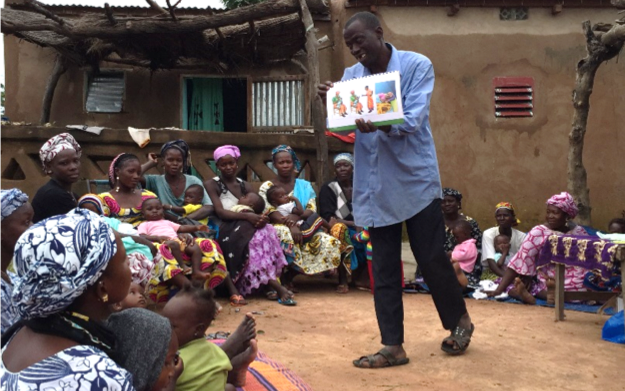
In Mali, the intervention was implemented through CHVs who were responsible for AM screenings (community delivery platform). Caregivers from both study groups with children aged 6-23 months were invited to attend monthly village-level meetings where CHVs screened the children and delivered BCC. Intervention caregivers were given the SQ-LNS at the end of these sessions.
The impact of PROMIS
- In both countries, PROMIS increased acute malnutrition screening coverage by an impressive 20 to 40 percentage points, reaching 48% in Burkina Faso and 63% in Mali.
- Despite increased screening, PROMIS had no effect on acute malnutrition treatment coverage, which remained unacceptably low at the end of the program (24% in Burkina Faso and 5% in Mali).
- The impact on acute malnutrition was modest and seen only in Mali. PROMIS reduced the number of new cases (AM incidence) in Mali by 29%, but no effect was found on the prevalence of acute malnutrition. The intervention also increased children’s weight-for-length Z-scores by 0.1. In Burkina Faso, however, no impact was found on either the incidence or prevalence of acute malnutrition.
- A far greater share of caregivers in Mali (73%) received monthly SQ-LNS than in Burkina Faso (47%). In Mali, CHVs sometimes distributed the SQ-LNS without organizing BCC sessions or conducting screenings. This was less of an issue in Burkina Faso, where the main constraint was that the scheduled BCC sessions were not always organized (as per intervention design).
Lessons learned for CMAM programs
By integrating preventive interventions into AM screening, PROMIS achieved one of its main goals—to significantly increase screening coverage. IFPRI’s study found that the SQ-LNS provided a strong incentive in both Burkina Faso and Mali for caregivers to attend monthly screenings. Yet the lack of impact on AM treatment suggests that there are still barriers preventing children identified as suffering from AM from being referred to, enrolled in, and treated by a CMAM program.
The evaluation also revealed tradeoffs between delivery platforms. Community-based platforms, like the one used in Mali, may be particularly effective at addressing two important barriers to caregivers’ participation: Distance to services and the opportunity costs of caregivers’ time. But health facility delivery platforms, like the well-baby consultations used in Burkina Faso, may provide higher-quality services and better adherence to program implementation guidelines. The well-baby consultations also have the potential to serve as a “one-stop shop” that provides caregivers with other preventive and curative clinical services during their visits for AM screening.
Is there a way to combine the benefits of both platforms to increase treatment coverage and reduce AM? Further research should test the operational feasibility and effectiveness of a community-based model that brings all elements of CMAM into a single community-level platform, thus easing the burden of participation for caregivers. Key to the success of such an approach will be to establish careful monitoring and supervision to ensure high-quality implementation and service delivery without overburdening the system.
Lieven Huybregts and Elodie Becquey are Research Fellows with IFPRI’s Poverty, Health, and Nutrition Division (PHND), Jef Leroy is a Senior Research Fellow with PHND, and Marie Ruel is Director of PHND; they were the principal investigators in the study. Tracy Brown is an IFPRI Senior Editor; she prepared the text of this post.
This work was supported by Global Affairs Canada (GAC) and the CGIAR Research Program on Agriculture for Nutrition and Health (A4NH) led by IFPRI.